Abstract
Objective: To describe demographic characteristics, clinical characteristics, and patterns of symptom management in patients undergoing oncology acupuncture. Methodology: A retrospective chart review of cancer patients who received acupuncture between May 2013 and April 2014. Setting: A regional, tertiary care academic medical center and National Cancer Institute (NCI)-Designated Cancer Center. Patients: 50 patients; 15 men and 35 women. Variables assessed: Gender, age, cancer diagnosis, treatment modalities received, primary symptom prompting acupuncture referral, and number of acupuncture treatments received. Results: Among 50 patients with cancer who were treated with acupuncture, 42 were diagnosed with a solid tumor and 8 with a hematologic malignancy. Neuropathy was the most common complaint prompting acupuncture treatment, followed by arthralgia and nausea. Of the patients with solid tumors, 19 were women diagnosed with breast cancer, all of whom had a primary symptom of neuropathy. The most common treatment administered for these women were taxanes and alkylating agents. Radiation therapy was strongly correlated with neuropathy. Conclusion: Among cancer patients who received acupuncture, breast cancer was the most common tumor type, with neuropathy being the most common chief complaint prompting acupuncture treatment.
Registration
The study obtained Institutional Review Board Approval (IRB00010921).
Introduction
Cancer therapy often causes myriad unwanted symptoms and side effects that lead patients to seek medical management for symptom relief. In 2017 more than 1.6 million people in the United States were diagnosed with cancer, most undergoing some form of surgery, chemotherapy, and/or radiation to treat their disease.1 Integrative medicine has been a welcome addition to conventional prophylactic and palliative standards of treatment, offering another avenue of clinical support.
Acupuncture in the oncology setting has been used in China for many centuries and, in recent decades, has become available as an integrative therapy in the Western medical culture. Our institution has adopted supportive care practices based on the success of numerous respected institutions. The addition of acupuncture as a treatment option at the Oregon Health and Science University (OHSU) has greatly enhanced oncology patient care, on a physical and psychosocial dimension.
A growing body of evidence supports the use of acupuncture for a multitude of symptoms patients frequently experience as a result of cancer itself or cancer treatment.
Over the past 20 years, acupuncture has gained a strong foothold in the medical community as an adjunct therapy for pain, infertility, neurological conditions, and cancer treatment–related side effects. Clinical research suggests the use of acupuncture in the oncology setting may be beneficial for symptoms and conditions such as post-chemotherapy fatigue,2,3 chemoradiation-induced nausea and vomiting,4-7 peripheral neuropathy,8 xerostomia,9-12 hot flashes,13-19 insomnia and anxiety,20 pain, and postoperative ileus.21-26
In the inaugural year of the OHSU oncology acupuncture service, we reviewed patient demographic and clinical characteristics to identify factors promoting the use of acupuncture. With these data, we will optimize symptom assessments to ascertain the clinical efficacy of acupuncture among subset populations who frequently use this service.
Methods and Materials
Upon institutional review board approval, we analyzed records of patients with a cancer diagnosis who elected to receive supportive acupuncture treatment between May 1, 2013 and April 29, 2014 at OHSU. A total of 50 patients were identified, with a majority (n=48) having received at least 1 primary oncologic treatment modality (surgery, chemotherapy, or radiation). Patients sought acupuncture for symptoms primarily related to cancer treatment–related side effects.
Initiation of acupuncture therapy came from either a physician referral or patient self-referral. Treatments were performed by a sole, licensed acupuncturist, in an outpatient clinical oncology setting. On each visit the acupuncturist reviewed patients’ charts for medical history, current course of treatment, and clinical updates. Current symptoms and complete review of systems were also assessed, along with tongue and pulse diagnosis.
A Traditional Chinese Medicine (TCM) diagnosis was determined by patient history, tongue, and pulse. Acupuncture points were selected based on standard TCM point prescriptions according to diagnosis and research-supported protocols. Needles were inserted and manipulated until de qi (a sensation experienced by the patient such as tingling, aching, or heaviness and a grasping sensation on the needle by the acupuncturist) was achieved. Depth of needle placement was generally 1 cun, traditionally defined as the width of the thumb at the knuckle or ~33.33 mm, or less with point placement on full body, auricular, and scalp. Needle retention was 20 to 30 minutes with manipulation of needles after 10 to 15 minutes with even, reinforcing, or reducing techniques to reinvigorate the de qi sensation.
Variables selected for data acquisition and analysis included patient demographics, which included gender and age; cancer type; treatment modalities; chemotherapy class; and type and number of symptoms prompting acupuncture referral. Inferential statistical analysis was limited to a stepwise logistic regression model to determine significant contributors to symptoms leading to acupuncture use.
Results
Acupuncture utilization among oncology patients
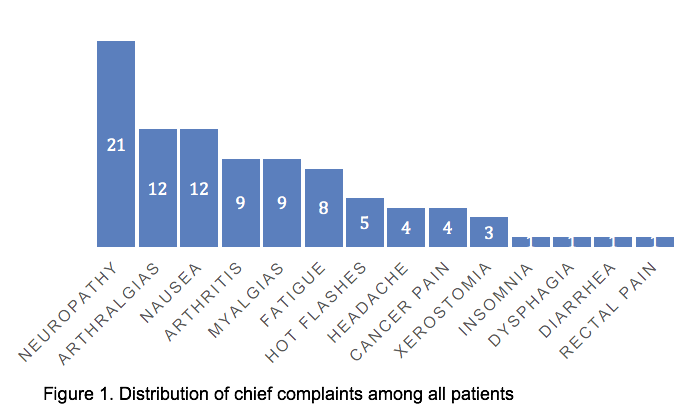
A total of 50 patients (median age 59; interquartile range [32-80]) received acupuncture, with more women (n=35; median age 59) than men (n=15; median age 61). Forty-two (84%) of the cohort were diagnosed with a solid tumor while 8 (16%) had a hematologic malignancy. A majority of patients (n=40; 80%) requested acupuncture for 1 to 2 clinical complaints. Overall, cancer treatment–related neuropathy (n=21) was the most common complaint prompting acupuncture treatment, followed by arthralgia (n=12), and nausea (n=12; Figure 1). A majority of patients did receive chemotherapy (n=43; 86%) and there was no correlation between number of chemotherapy agents used and number of symptoms prompting acupuncture referral.
Acupuncture among radiation therapy patients
Among the 50 patients whose records were analyzed, 26 patients, including 8 men (median age 64) and 18 women (median age 59.5), received radiation therapy. Twenty-two patients also received chemotherapy, and 15 in the chemoradiation cohort underwent surgery (Table 1). Patients with breast cancer (n=11) were the most prevalent users of acupuncture, followed by patients with head and neck (n=4) and lung cancer (n=3). Most patients (n=20) requested assistance with 1 to 2 symptoms, with the most common symptoms being neuropathy (n=6), arthralgias (n=6), and nausea (n=6). Among breast cancer patients who underwent radiation, the most common chief complaints were arthralgias (n=6), myalgias (n=5), and neuropathy (n=4), and the most commonly used chemotherapy were taxanes (n=9). The median number of complaints (n=1.5) for which patients requested acupuncture did not differ among those who underwent mastectomy vs lumpectomy followed by radiation. Among radiation therapy patients who received an aromatase inhibitor alone for adjuvant endocrine therapy, there were more symptoms for which the patient requested acupuncture referral than among patients who received tamoxifen alone (Table 2). Stepwise linear regression found radiation, apart from other therapeutic modalities, was mainly responsible for neuropathy prompting acupuncture referral (P=0.0063).
Table 1. Frequency and Distribution of Radiation Therapy and Concurrent Treatment
| Treatment modality | Total number receiving modality | Men (%) | Women (%) |
| Radiation alone | 1 | 100 | 0 |
| Radiation + surgery | 3 | 0 | 100 |
| Radiation + chemotherapy | 7 | 43 | 57 |
Table 2. Breast Cancer Radiotherapy Patients’ Surgical and Systemic Interventions
| Surgery | Endocrine Therapy | |||||
| Lumpectomy | Mastectomy | No endocrine therapy | Tamoxifen | AI | Tamoxifen + AI | |
| Number receiving modality | 8 | 4 | 5 | 3 | 2 | 1 |
| Median number of complaints prompting acupuncture referral | 1.5 | 1.5 | 3 | 1 | 3.5 | 1 |
Abbreviation: AI, aromatase inhibitor
Breast cancer patient subset analysis
Of the solid tumor patients, 19 (median age, 59; interquartile range [32-71]) were diagnosed with breast cancer, all of whom had a chief complaint of neuropathy. The most common treatment administered for these 19 women were taxanes (n=16; 84%) and alkylating agents (n=10; 53%). Fewer women with mastectomy than lumpectomy requested acupuncture referral.
Discussion
Few studies have examined the overall application of acupuncture in the oncology setting. Though this study is small, we believe by identifying areas of utilization in specific demographics and symptom management we will shed light on patient needs for which they are seeking assistance in their cancer experience.
It is estimated that between 1.7% and 31% of patients with cancer have used acupuncture as a therapeutic treatment.27-29 A 2007 study examining acupuncture use among American adults revealed that 65% of the 344 individuals who had recently used acupuncture were women.30 Women tend to be more frequent users of complementary and alternative medicine (CAM), with breast cancer patients being the most consistent users of CAM compared to women with other tumor types.29,31,32
The use of acupuncture to treat women with breast cancer for common symptoms such as hot flashes, arthralgias, and nausea has been a focal area of acupuncture research. Climacteric “hot flash” studies have shown a decrease in hot flash scores, with secondary improvements in mood, sleep quality, and overall quality of life. In our study, breast cancer patients were the most prevalent users of acupuncture looking for support with the aforementioned symptoms with the addition of neuropathy.
Small studies suggest acupuncture reduces symptoms of chemotherapy-induced peripheral neuropathy, with improvements seen in function, nerve conduction, and neuropathic pain.8,33-37 Neuropathy is a difficult symptom to treat, and standard medications used to relieve the pain and discomfort often create unwanted side effects. Acupuncture for aromatase inhibitor–induced arthralgia in women with breast cancer has also been proven effective as an analgesic aid.21,22 Patients often welcome the additional option for pain relief without the side effects commonly seen from pain-relieving medications.
Patients with head and neck cancers frequently receive a combination of chemoradiation as part of their cancer treatment. Xerostomia and nausea are common side effects experienced in this population due to the area of treatment and local tissue changes in the oral cavity and throat. Acupuncture has been well-documented to help with nausea and vomiting related to chemotherapy4-7 and radiation.38 Compounding effects of oral dryness create added barriers to proper hydration, nutrition, and overall oral health throughout the course of treatment and thereafter. Utilizing acupuncture as a therapeutic treatment to minimize nausea and xerostomia can minimize overall toxicity of treatments, helping support a full course of therapy.9
Seeking out integrative therapies to manage symptoms is certainly a growing trend among patients with cancer. With many patients receiving a combination of care that includes chemotherapy, radiation and surgery, there are many opportunities for acupuncture use along the spectrum of care. Within our radiation cohort, more than half received all 3 cancer treatment modalities. Each treatment modality produces different side effects that acupuncture may help manage throughout the continuum of care. Acupuncture, increasingly available in the oncology setting, is a safe and effective treatment that can offer the additional support patients are looking for to manage symptoms associated with cancer and cancer treatment.









